Glaucoma
All info about glaucoma
What is glaucoma?
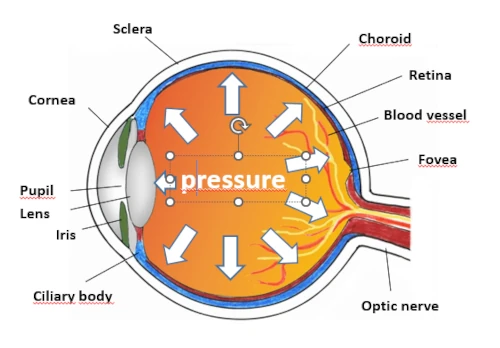
Glaucoma is an eye disease that is often accompanied by increased intraocular pressure. It is one of the most common causes of blindness worldwide. In Germany alone, around half a million people suffer from glaucoma, although experts estimate that the actual number is much higher due to the number of unreported cases. Around one-tenth of all people with glaucoma end up with serious vision impairments, but almost none will be completely blind.
The increased pressure inside the eye occurs when the fluid circulating in the eye does not drain properly, which then reduces blood flow to the retina and optic nerve. For example, as soon as the pores of the drainage tubules become clogged, the intraocular pressure increases, and excess fluid accumulates in the eye. At the same time, the blood flow in the optic disc decreases, reducing the supply of oxygen and damaging the optic nerve. In so-called “normal pressure glaucoma,” the eye pressure is normal, but vision loss can still develop and slowly progress over time. The cause of this kind of glaucoma is that blood vessel regulation is impaired, that is, the vessels are too thin to transport sufficient oxygen and glucose, which in the long run can also impair vision.

“The optimization of residual vision is a holistic complement to ophthalmological care such as eye drops or surgeries. We continue where ophthalmology stops. We combine conventional medical science with new findings from modern brain research and traditional medicine methods.”
Causes of glaucoma
Anything that increases the pressure inside the eye and/or decreases the blood flow in the optic disc can lead to glaucoma. In addition to increased intraocular pressure, these risk factors are also known to lead to glaucoma:
For example, if a person’s blood flow is continuously very low or fluctuates widely this can reduce eye function. This is the reason why glaucoma patients’ hands and feet may often feel cold, and other conditions such as migraine or tinnitus can occur. Genetic predisposition, such as a thin cornea, plays a role, as does ethnicity, because people with darker skin develop glaucoma more often than those with lighter skin. The risk of developing glaucoma also increases with age, especially in people who are under constant stress or plagued by a lot of worries, anxiety, or perfectionism.
Different forms of glaucoma
The following types of glaucoma are the most common.
Secondary glaucoma
Secondary glaucoma can develop as a result of an injury or another eye disease, such as a tumor inside the eye. Sometimes certain medications cause glaucoma, as do vascular occlusions, eye infections, and cataract surgery.
Open-angle glaucoma
Open-angle glaucoma is the most common. It is characterized by increased eye pressure due to excess aqueous humor being produced in the eye that cannot drain away. But many patients have glaucoma even though their eye pressure is normal . Here, a lack of blood supply leads to a condition called “vascular dysregulation,” which paralyzes the nerve cells in the retina but does not cause them to die.
Narrow angle glaucoma
In narrow angle glaucoma, which is relatively rare, the outflow of aqueous humor is completely obstructed. If this phenomenon happens very suddenly, it is called a glaucoma attack.
Glaucoma emergencies
A glaucoma attack is an absolute emergency, because if the aqueous humor outflow is suddenly blocked completely, a strong pressure builds in the eye. The eyeball becomes hard, and patients may suffer from reddened or painful eyes, nausea, and vomiting. Even severe headaches and cardiac arrhythmias are possible. The pupil may no longer respond to an incidence of light. Often, there is then a sudden loss of vision in one eye.
How can glaucoma be prevented?
As with all diseases, it is best to detect glaucoma as early as possible. To diagnose glaucoma in time, patients should have regular examinations by an ophthalmologist (eye doctor). If glaucoma is detected at an early stage, progression of the disease can be prevented or significantly slowed.
The general recommendation is to have a regular check-up examination every three years starting from the age of 40 and every year after age 60. Those who are genetically predisposed to develop glaucoma should watch out for possible symptoms and consult an ophthalmologist at the first signs of vision problems.
This also applies to patients under age 40 whose eye has been injured or even bruised. They should visit the ophthalmologist once a year to have their intraocular pressure measured.
In general, a health-conscious lifestyle helps to prevent eye diseases such as glaucoma. Patients should not smoke, for example, because nicotine worsens blood flow to the optic nerve. They should drink 2 liters (8 cups) of water daily, regularly exercise, and try reducing their worries and stress. To help their nerves and blood vessels to stay healthy, patients should follow a healthy diet or take supplements to maintain a sufficient supply of omega-3 fatty acids, Q10, and lutein, all of which are essential for the health of the retina.
How is glaucoma diagnosed?
To diagnose glaucoma, the intraocular pressure is first measured. For this purpose, the cornea is anesthetized and an applanation tonometer measures the force required to mechanically flatten the cornea. Eye pressure also can be measured without contact using pneumotonometry, which works with tiny puffs of air. In addition, the corneal thickness is measured, as it influences the measured pressure values. Because the pressure values may fluctuate over the course of a day, it may be necessary to repeat measurements to create a daily pressure profile.
Intraocular pressure alone is not enough to make a diagnosis of glaucoma. Other tests must be performed, such as a visual field examination (perimetry). For this test, the patient sits in front of a perimeter with one eye covered. While the seeing eye fixates on a central specific point, small dots of light appear at different positions on the visual field. Whenever the patient sees one of these lights, their task is to press a button. In this way, any impairment of the patient’s vision can be detected.
The ophthalmoscopy may also be used to determine the size and shape of the optic nerve head at the optic disc cavity. In glaucoma, a pale optic disc is often observed, which is a sign of lack of blood flow or even degeneration of the nerve. A slit lamp can be used to detect deposits in the eye, such as pigments or proteins, as well as possible abnormalities of the chamber angle in glaucoma.
Vision with glaucoma
The high intraocular pressure caused by glaucoma is painless and usually goes unnoticed for a long time. However, the pressure can cause the cornea to swell. As a result, the person can sometimes see colored rings spreading around light sources.
If large parts of the optic nerve become inactivated or destroyed, visual field loss occurs, which can lead to total blindness (though this is very rare nowadays). In this case, an object can still be recognized, but the object next to it can no longer be recognized. Patients have to test each eye separately, because asymmetric visual loss of both eyes is not noticed by the brain, since the brain constructs an overall picture from both eyes. A reduced field of vision can lead to difficulties in driving or problems with reading, climbing stairs, or recognizing faces. And it can lead to overall foggy vision.
Glaucoma treatment
Once glaucoma has been diagnosed, it must be treated and monitored closely to prevent the patient from going blind. The ophthalmologist will set an individual target value for the intraocular pressure. This value is used to find the optimal therapy that can prevent progression of the disease. It is also important to control the patient’s blood pressure. If the patient suffers from high blood pressure and takes appropriate blood pressure-lowering medication, it is possible that their blood pressure will drop too much at night and their optic nerve will no longer be supplied with sufficient blood and nutrients.
Medications: Eyedrops
Glaucoma is initially treated with eyedrops that contain drugs, designed to lower intraocular pressure. There is a whole range of different drugs, some of which have quite different mechanisms of action. If necessary, they can be combined with each other. The active substances contained in the eyedrops are miotics, beta blockers, carbonic anhydrase inhibitors, prostamides, and prostaglandins. The eyedrops must be used for life following a doctor’s instructions. They can have quite unpleasant side effects and can irritate the eye. Itching and redness are often reported. Beta-blockers can have systemic effects on other organ systems, such as stressing the respiratory or cardiovascular systems.
Nutritional supplements
There are several nutritional supplements that support eye health. See “Eye Health” for details.
Glaucoma surgery
There are several glaucoma surgery options available. The procedure chosen in each case depends on the individual diagnosis and the cause of the disease. The goal of all surgery methods is to permanently lower intraocular pressure by enhancing the fluid drainage of the eyes. Surgical interventions can have risks, and patients need to discuss these with their eye doctor.
SAVIR therapy for glaucoma
Vision loss following optic nerve damage was long considered to be permanent. However, modern research has shown that vision loss can be improved and partially recovered with the help of SAVIR therapy. This has been confirmed by several clinical studies. In SAVIR therapy, small microcurrent pulses activate blood flow in the eye and brain, so that “silent” nerve cells can be reactivated and vision can be improved. In a clinical trial, 82 patients whose visual performance was limited by optic nerve damage were treated for 10 days either with microcurrent (SAVIR therapy) or with a noncurrent placebo therapy. For the microcurrent treatment, electrodes were attached near the eyes, and the patients were administered very mild microcurrent pulses via the electrodes for 40 minutes daily. After only 10 days of microcurrent therapy, visual performance improved significantly in two-thirds of the study participants, as the neuron network in their brains had recovered. Blood flow to the brain also improved. In one example of this recovery, the visual cortex in the back of the head was once again able to exchange signals with the frontal cortex in the forehead area in order to generate meaningful images from the visual impulses of the eyes. As a result, patients were able to see better, even though the damage to the optic nerve was considered irreparable. The therapy had simply reactivated previously “silent” neurons.
Risks and side effects of SAVIR therapy for glaucoma (green star)
Risks and side effects of SAVIR therapy are rare and only mild. The current pulses, which are significantly lower than those of a pacemaker, are so weak that they are hardly felt on the skin. Patients may notice brief flashes of light when their eyes are closed during treatment.
Worldwide Unique, Holistic Therapy for Optic Nerve Damage
0
Years of Research Leadership
Years of Experience and Success in Treating Patients